Muscle metabolism disorders: equine polysaccharide storage myopathy (PSSM)
PSSM is currently a hot topic in the equestrian world. But what’s the story behind these four letters? - An overview.Access denied: When muscles can’t access their stores
Muscle cells build up glycogen stores to have energy on hand for muscle work. Glycogen is a complex carbohydrate made up of many small blood sugar molecules (glucose). In PSSM, the glycogen build-up and breakdown processes are altered.Horses with PSSM build up glycogen in certain muscle fibres faster than healthy horses do. However, the excess glycogen stores can no longer be used to produce energy, as the breakdown into glucose is no longer possible. The overloading of the muscle cells with glycogen and the lack of access cause problems for affected horses; these problems will be discussed below.
It is now known that this muscle metabolism disorder has various causes, and so it is generally separated into two types: Type 1 PSSM and Type 2 PSSM. Scientists have been able to clarify that Type 1 PSSM involves a certain genetic mutation causing impaired glycogen metabolism. However, there are also horses without this mutation with muscle cells clearly overloaded with glycogen. They thus show a similar clinical picture, but the cause is different. These cases are called Type 2 PSSM, involving one or more diseases, the exact cause of which has not yet been scientifically determined.
Type 1 PSSM: genetic mutation with consequences
In Type 1 PSSM, a genetic mutation causes changes to the structure of a glycogen-building enzyme (glycogen synthase 1, or GYS1). Here, the enzyme operates differently than in horses without Type 1 PSSM. Both alleles of the gene can be affected if just one parent has passed on the genetic mutation (heterozygous PSSM1 carrier) or both alleles if both parents have passed on the mutation (homozygous PSSM1 carrier). In both cases, the horse’s muscle metabolism changes, with homozygous PSSM horses exhibiting severe forms of the disease.Horses with Type 1 PSSM may experience a general drop in performance, muscle weakness, muscle atrophy, tight muscles, stiffness, changes in gait, lameness, and the most-dreaded consequence of all: equine rhabdomyolysis syndrome. This is because overloading the muscle cell with glycogen causes pain and can also lead to death of individual muscle cells. Blood work often shows increased muscle enzyme activity in horses with Type 1 PSSM, often even at rest.
The danger of a glycogen overloading arises when affected horses consume lots of easily digestible carbohydrates like starch or sugar, resulting in a rise in blood sugar levels, and the muscle cells absorb some of the excess blood sugar and store it in glycogen. Also problematic for affected horses are sudden, high performance demands – because even if part of their glycogen stores cannot be broken down normally, this does not apply to the entire glycogen of the muscle. If strenuous muscular effort causes a depletion of these normally depletable stores, there will be increased formation of new glycogen during the regeneration phase, with abnormal glycogen forming again and overloading the muscle cells.
There is now a simple genetic test to determine whether a horse suffers from Type 1 PSSM. This test requires only a blood or hair root sample. Such a test is advised when, for example, a horse shows signs of PSSM or when blood work shows increased muscle enzyme activity that cannot be explained by physical effort.
Testing is also important for stallions and mares used in breeding if the genetic defect is common in the breed. This includes Quarter Horses, Paint Horses, many draught breeds, Haflingers, and Cobs. Affected horses should not be used for breeding purposes.
Type 2 PSSM: from (yet) unknown cause(s)
Not all horses showing signs of PSSM test positive in genetic tests. If a horse has recurring acute muscular problems but no mutation of the GYS1 gene, the horse owner is initially presented with a puzzle. What now? The horse appears ill and everything points to PSSM, but the horse is not a carrier of the mutated GYS1 gene.Meanwhile, there are now other genetic tests offered on the market. However, it must be emphasised that these tests have not yet been validated and the current scientific data suggests that they are not suitable for diagnosing Type 2 PSSM. But what does that mean, specifically?
To understand, we need to take a look at the gold standard for diagnosing Type 2 PSSM: the examination of a muscle biopsy. Under a microscope, glycogen that has been abnormally stored in the muscle cells can be made visible. Pathologists can assess whether a horse has a healthy or pathologically altered glycogen metabolism by looking at the distribution and amount of glycogen in the muscle cells. According to the latest findings, the horse need not show strong clinical signs at the time of the muscle biopsy. Because the muscle cell will show changes even if there were problems in the past that aroused suspicion of PSSM. The body cannot break down the abnormally accumulated glycogen and destroyed muscle cells can no longer regenerate. In other words, once the damage occurs, it’s permanent.
Genetic tests for Type 2 PSSM involve the examination of several genes and their possible alleles. However, there is no proof as to whether certain alleles are actually associated with altered muscle metabolism (or simply represent possible genetic variance). Differences in genotypes do not automatically mean that an individual is sick. In its genes for determining colour, a chestnut horse will have different alleles than a bay, but this is in no way connected to disease. Just considering the differences in appearance and performance of the musculature of different horse breeds, a wide variance in genes involving muscle is also likely between horses without disease.
So far, studies on tests for Type 2 PSSM also tend to confirm the view that the detectable deviations in the genotypes are not associated with a muscle metabolism disease. For example, the frequency of testing genetically positive for Type 2 PSSM is similar in both horses with normal muscle biopsies and no signs of disease as well as in horses that test positive for PSSM through muscle biopsies. Therefore, a muscle biopsy should still be performed if Type 2 PSSM is suspected.
Conversely, this does not mean that it is impossible to develop a validated genetic test for Type 2 PSSM in the future, because it is still possible that Type 2 PSSM is also a genetic disease or diseases. However, more research is needed to find out which mutations might actually be responsible.
Diet, management, and training for PSSM horses – what to consider
The good news: with good management, many horses can lead almost problem-free lives and be willing recreational sport partners despite having PSSM. There are a few things horse owners should keep in mind.Horses with Type 1 PSSM should consume very little starch and sugar through feed in order to keep the body’s glycogen production under control. Cereals and cereal products like oats, barley, maize, and rice bran therefore make unsuitable concentrates for affected horses. Make sure that the sugar content of the forage is not too high as well. Most horses with Type 1 PSSM have no problems eating hay from mid-cut first cuttings.
But sugary hay that’s been harvested too early or even young pasture grass can lead to problems, especially if the horses are not in work every day and consume more than they actually need. If a horse with Type 1 PSSM has problems despite being fed a cereal-free diet, you should take a look at the forage supply and, if possible, replace part of the hay ration with straw. You should also minimise pasture grass consumption, for example by using a feed brake or even by substituting pasture time with paddock grazing only.
If forage alone is not sufficient for a horse with Type 1 PSSM to maintain its weight easily, you can also provide cereal-free concentrates that are low-sugar and low-starch. Oils are also an option. A concentrate feed’s protein content can be somewhat higher to counteract any muscle loss.
To optimally support the muscles, you should also make sure to supply all the nutrients relevant for the muscles in sufficient amounts. For example, your mineral feed should have enough selenium and vitamin E to cover requirements and prevent deficiencies. Magnesium is also essential for the function of many enzymes in muscle tissue, so a sufficient supply is essential. Essential amino acids are also important for horses with Type 1 PSSM, as they are important building blocks for muscle protein.
At the moment, similar feed recommendations apply to horses with Type 2 PSSM, although there is evidence that not all horses with Type 2 PSSM have problems from sugar or starch consumption. But because a cereal-free diet that’s low in easily digestible carbohydrates is good for all horses, there is actually no reason to risk problems due to starch or sugar. Other recommendations for horses with Type 2 PSSM, such as feeding excessive amounts of protein, have not been substantiated. A prolonged, excessive oversupply of protein should be avoided due to the considerable strain it will put on the liver and kidney metabolism.
The husbandry and training of horses with PSSM can be adapted in order to keep their glycogen metabolism as "calm" as possible. Ideal types of husbandry involve systems where the horses are almost constantly moving and their feed rations are divided into several small portions over the course of the day (e.g. in an active stable or a Paddock Paradise). With regard to training, care should be taken to give affected horses light exercise every day if possible, but avoiding exertion peaks. Long slow distance work, primarily at a walk with intervals of increasing cross-country trot and canter, is ideal for affected horses. In the school, light gymnastic work is recommended – if the horse resists, always consider the underlying disease and that pain is a possible trigger. In most cases, there is no impediment to your horse leading a contented life as an active leisure horse.
AGROBS products for PSSM horses:
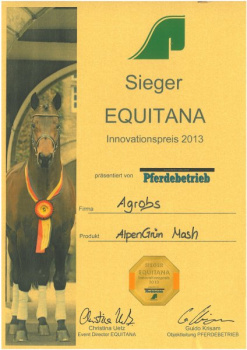
- AlpenGrün Müsli, AlpenGrün Mash, and AlpenGrün Seniormüsli are cereal-free concentrates containing pre-caecal digestible protein for horses with increased energy requirements
- Omega3 Pur delivers needed energy and contains no starch or sugar
- Amino Pur contains methionine, lysine, and threonine (important essential amino acids for muscle) and has no cereals or added sugars
- Gipfelstürmer Mineral contains micronutrients important for muscle like selenium, vitamin E, and amino acids in highly available form and also has no cereals or molasses
- Selen Pur can effectively compensate for inadequate selenium and vitamin E in the ration
- Magnesium Pur combines 3 sources of magnesium for the best possible supply.
Celina Hofmann, Veterinary Surgeon
July 2022, © AGROBS GmbH
Sources:
- Borgia, L., Valberg, S., McCue, M., Watts, K., & Pagan, J. (2011). Glycaemic and insulinaemic responses to feeding hay with different non-structural carbohydrate content in control and polysaccharide storage myopathy-affected horses. Journal of Animal Physiology and Animal Nutrition, 95(6), 798–807. https://doi.org/10.1111/j.1439-0396.2010.01116.x
- Coenen, M.; Vervuert I.: Pferdefütterung. Georg Thieme Verlag KG, Stuttgart, 2020
- Geor, R.J.; Harris, P.A., Coenen, M.: Equine Applied and Clinical Nutrition: Health, Welfare and Performance. Saunders Elsevier, 2013
- Johlig, L., Valberg, S. J., Mickelson, J. R., Klukowska, J., Reusser, H. R., Straub, R., & Gerber, V. (2011). Epidemiological and genetic study of exertional rhabdomyolysis in a warmblood horse family in Switzerland. Equine Veterinary Journal, 43(2), 240–245. https://doi.org/10.1111/j.2042-3306.2010.00161.x
- McCue, M. E., Anderson, S. M., Valberg, S. J., Piercy, R. J., Barakzai, S. Z., Binns, M. M., Distl, O., Penedo, M. C., Wagner, M. L., & Mickelson, J. R. (2010). Estimated prevalence of the Type 1 Polysaccharide Storage Myopathy mutation in selected North American and European breeds. Animal Genetics, 41 Suppl 2, 145–149. https://doi.org/10.1111/j.1365-2052.2010.02124.x
- Naylor, R.J. (2015), Polysaccharide storage myopathy – the story so far. Equine Veterinary Education, 27: 414-419. https://doi.org/10.1111/eve.12329
- Valberg SJ, McCue ME, Mickelson, JR. The Interplay of genetics, exercise and nutrition in polysaccharide storage myopathy. Journal of Equine Veterinary Science, 2011;31:205-210. https://doi.org/10.1016/j.jevs.2011.03.001
- Valberg et al 2020 Commercial genetic testing for type 2 polysaccharide storage myopathy and myofibrillar myopathy does not correspond to a histopathologic diagnosis. Equine Veterinary Journal. https://doi.org/10.1111/evj.13345
- Williams et al 2020, Candidate gene expression, coding sequence variants and muscle fiber contractile force in Warmblood horses with myofibrillar myopathy, Equine Veterinary Journal https://beva.onlinelibrary.wiley.com/doi/10.1111/evj.13286